contamination colonisation infection
|
Colonization v Infection
Contamination: Presence of a microorganism on a body surface or an inanimate object Carrier A carrier is an individual that harbors a specific microorganism in the absence of discernible clinical disease and serve as a potential source of infection A carrier may be an individual who is: colonized |
|
Infection vs Colonization
Colonization: Definition The presence of a microorganism on/in a host with growth and multiplication of the organism but without interaction between host and organism (no clinical expression no immune response) You wouldn’t know it was there unless you looked for it (via lab tests) |
|
Wound infection in clinical practice An international consensus
PRODUCTION: Alison Pugh DESIGNER: Jane Walker PRINTED BY: Printwells Kent UK FOREIGN TRANSLATIONS: RWS Group London UK The content of this document has been carefully considered to relate directly to daily clinical practice In particular it provides broad clear and safe guidance on the areas of diagnosis and the topical/systemic treatment of |
What is the difference between colonization and infection?
colonization and infection is that colonization is the process of establishment of the microbe in the body tissues while the infection is the process of invading body tissues by the microbe to cause the symptoms of the disease.
What is meant by infection and colonization?
Colonization. • Indicates the presence of an organism without symptoms of illness. It can occur in the nares, trachea, skin folds, rectum, or in an open wound such as decubitus ulcer. The patient does not have symptoms when colonized. Infection indicates the presence of an organism with clinical signs and symptoms of illness.
What is bacterial colonization and what causes it?
Colonization of the upper airway is the prerequisite to invasive disease by many respiratory tract pathogens. Colonization drives evolution of virulence factors that cause disease. Colonizing bacteria must adhere to the mucosal surface, obtain nutrients for growth, evade host immunity, and transmit to a new host.
Lisa MacGregor Wound infection continues to be a challenging problem and represents a considerable
PRODUCTION: Alison Pugh DESIGNER: Jane Walker PRINTED BY: Printwells, Kent, UK FOREIGN TRANSLATIONS: RWS Group, London, UK The content of this document has been carefully considered to relate directly to daily clinical practice. In particular, it provides broad, clear and safe guidance on the areas of diagnosis and the topical/systemic treatment of
PRINCIPLES OF BEST PRACTICE
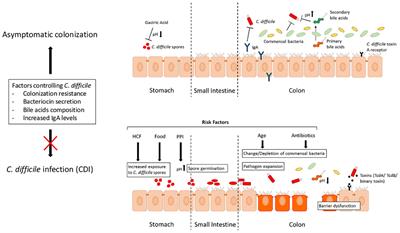
Even though it is virtually inevitable that most wounds contain micro-organisms, many heal successfully. However, sometimes micro-organisms (particularly bacteria) multiply, invading and damaging tissues, delaying healing and occasionally causing systemic illness. The potential for bacteria to produce harmful effects is influenced by the: ability o
DEFINITIONS
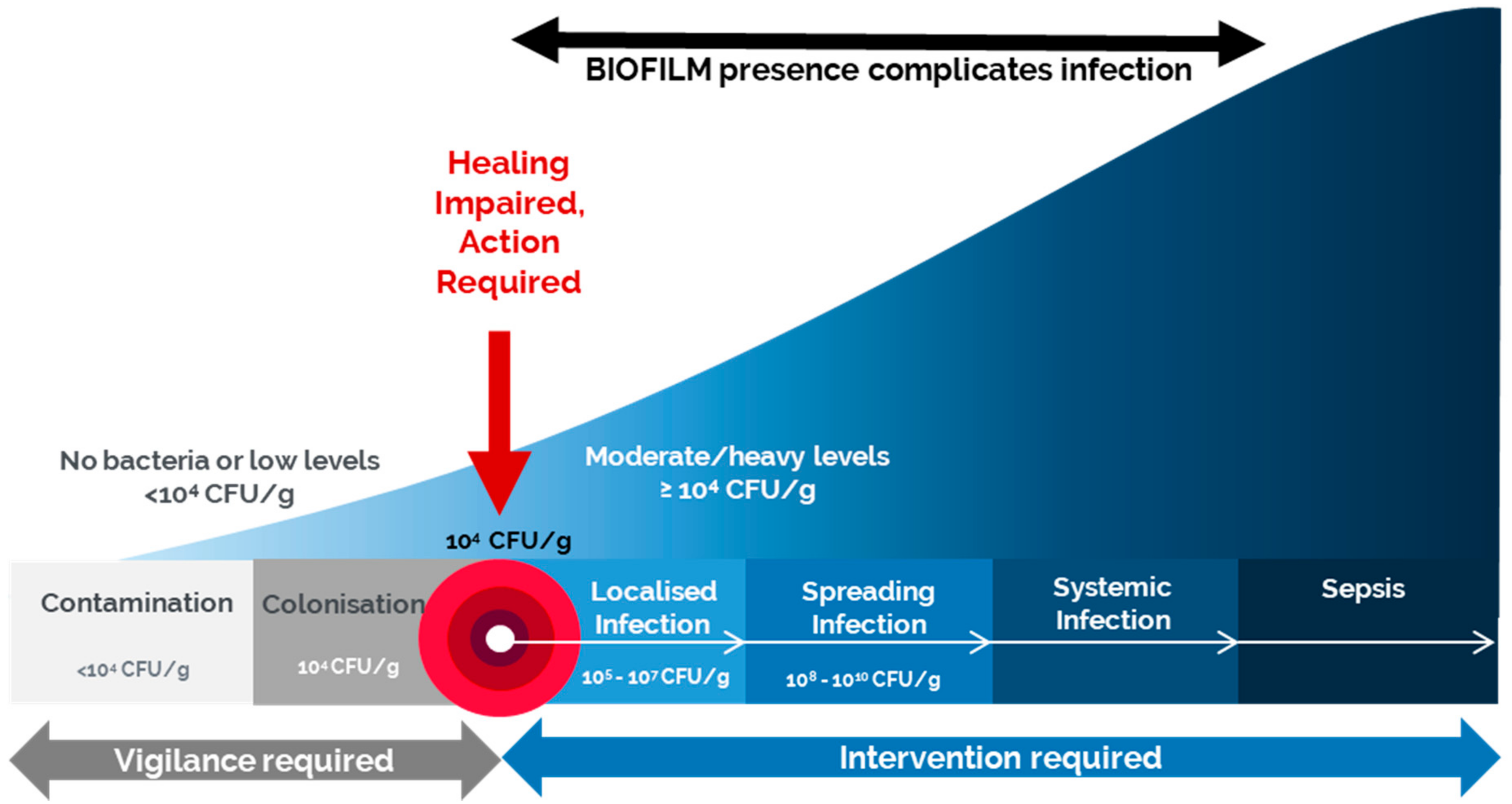
The presence of bacteria in a wound may result in: contamination – the bacteria do not increase in number or cause clinical problems colonisation – the bacteria multiply, but wound tissues are not damaged infection – the bacteria multiply, healing is disrupted and wound tissues are damaged (local infection). Bacteria may produce problems nearby (sp
Intervention required
*Localised infection may or may not be accompanied by the classical signs and symptoms of inflammation. When it is not, various terms have been used, eg critical colonisation (see main text) ? Further research is required to fully understand the factors involved in the transition from colonisation to localised infection. This may facilitate future
APPLICATION TO PRACTICE
Intervention is usually required only when the patient is at a high risk of wound infection (see page 2) or when the interaction between the bacteria in a wound and the host’s defences impairs healing, causes further damage, and results in localised, spreading or systemic infection woundinfection-institute.com
DIAGNOSIS
Figure 2 Pocketing Smooth, non-granulating areas in the The diagnosis of wound infection is made mainly on clinical grounds. Assessment should include evaluation of the patient, the tissues around the wound and the wound itself for the signs and symptoms of wound infection, as well as for factors likely to increase the risk and base of a wound su
RISK OF INFECTION
The risk of wound infection is increased by: any factor that debilitates the patient, impairs immune resistance or reduces tissue perfusion, eg: – comorbidities – diabetes mellitus, immunocompromised status, hypoxia/poor tissue perfusion due to anaemia or arterial/cardiac/respiratory disease, renal impairment, malignancy, rheumatoid arthritis, obes
MANAGEMENT
Effective management of wound infection often requires a multidisciplinary approach and may involve specialist referral (Figure 5). It aims to readjust the interaction between the patient and the infecting micro-organism(s) in favour of the patient by: optimising host response reducing the number of micro-organisms. woundinfection-institute.com
OPTIMISING HOST RESPONSE
Implementation of measures to optimise host response will enhance the ability of patients to fight infection and improve their healing potential. Systemic factors that may have contributed to the development of the wound infection (and often in the case of chronic wounds, the wound itself) should be addressed, eg optimisation of diabetic glycaemic
Effective hygiene and preventative measures
Infection control procedures should be followed to prevent further contamination of the wound and cross-contamination. Good hygiene practice includes paying particular attention to thorough hand cleansing/disinfection and suitable protective working clothes, including gloves. Figure 5 Effective management of wound woundinfection-institute.com
OPTIMISE HOST RESPONSE
Optimise management of comorbidities, eg optimise glycaemic control in diabetic patients, enhance tissue perfusion/oxygenation Minimise or eliminate risk factors for infection where feasible Optimise nutritional status and hydration Seek and treat other sites of infection, eg urinary tract infection woundinfection-institute.com
GENERAL MEASURES
Manage any systemic symptoms, eg pain, pyrexia Provide patient and carer education Optimise patient cooperation with management plan Ensure psychosocial support woundinfection-institute.com
RE-EVALUATE REGULARLY
Relate frequency of re-evaluation to the severity of the infection and condition of the patient Are the wound and patient improving? Is the wound starting to heal? If not, re-evaluate the patient and wound and adjust management accordingly Systematic monitoring and recording of symptoms is helpful in detecting improvement or deterioration. Consider
Cleansing infected wounds
Infected wounds should be cleansed at each dressing change. Cleansing by irrigation should use sufficient pressure to effectively remove debris and micro-organisms without damaging the wound or driving micro-organisms into wound tissues. ? The ideal agent for and method of cleansing infected wounds have not yet been identified. However, there may b
Antimicrobial therapy
Antimicrobial therapy may be required when other methods of reducing wound bacterial load are likely to be insufficient in localised infection, or when the infection is spreading/systemic. Antimicrobial agents – including antiseptics and antibiotics – act directly to reduce numbers of micro-organisms: Antiseptics are applied topically and are non-s
APPLICATION TO PRACTICE
Prompt, effective management of wound infection may reduce time to healing and minimise impact on patients, healthcare systems and society Treatment of an infected wound should follow a clear, decisive plan Management of comorbidities may require specialist input Good hygiene, wound debridement and wound cleansing will aid reduction in wound bacter
USING ANTISEPTICS
Antiseptics generally have a broad spectrum of antibacterial activity. Their action at multiple sites within microbial cells reduces the likelihood of bacteria developing mechanisms to avoid their effects and so may explain their relatively low levels of bacterial resistance. Factors influencing the choice of antiseptic for an infected wound includ
Roles and formulation
Antiseptics are used mainly in the treatment of infected open acute and chronic wounds (Box 3, see page 7). If there are signs of spreading or systemic infection, antiseptics should be used in conjunction with systemic antibiotics. Antiseptics are available in many different forms: liquids, pastes, creams, ointments, gels, powders, sprays and impre
APPLICATION TO PRACTICE
Treatment of infected wounds with antiseptics is often necessary – clearly define reasons for use, treatment goals and duration of use Use antiseptics in the context of a management plan that incorporates optimising host immune response and other methods of reducing bacterial load (Figure 5, see page 5) Consider how the formulation of an antiseptic
PRINCIPLES OF BEST PRACTICE
BOX 5 Useful definitions Argyria – A term that is often misused. This very rare condition produces blue-grey discolouration of the skin and is associated with long-term systemic exposure to silver salts. Argyria differs from the reversible local discolouration that may be associated with silver dressings; argyria is irreversible and can affect th
|
Infection v. Colonization
A carrier may be an individual who is: • colonized. • infected and asymptomatic. • in incubation period before disease. • convalescent from acute disease. The |
|
Infection ou Colonisation: une source importante du mésusage
contamination : mise en évidence de microbes non présents dans le site prélevé. • colonisation : présence de microbes sans infection associée. |
|
UNDERSTANDING WOUND INFECTION AND COLONISATION
The first step to understanding wound colonisation and infection is recognising that all wounds are contaminated with micro- organisms; contamination is the. |
|
MRGN – MULTI-RESISTANT GRAM-NEGATIVE BACTERIA
contaminated food may also result in the colonisation of the intestinal tract An MRGN infection can cause various symptoms depending on the location of ... |
|
Reflection paper on meticillin-resistant Staphylococcus
04.02.2011 Contamination colonisation and infection: animals and humans can be contaminated |
|
Hygienemaßnahmen zur Prävention der Infektion durch
22.03.2018 2.3.3 Kolonisation. 2.3.4 Dauer der Besiedelung. 2.3.5 Nosokomiale Infektion. 2.4 Outcome von Enterokokken-Infektionen in Abhängigkeit von ... |
|
Empfehlungen zur Prävention und Kontrolle von Methicillin
men zur Infektionsprävention auf die ent- Kolonisation oder -Infektion [178 195] |
|
Assessment of the Public Health significance of meticillin resistant
Food may be contaminated by MRSA (including CC398): eating and handling contaminated between infection colonisation and contamination from skin sites. |
|
Elimination of carriage
bacterial infections. Contamination of the patient. Sickness and disease. Dissemination intestinal colonisation. 3. Anti GN pipe-line dried. |
|
Environmental contamination makes an important contribution to
frequently touched by healthcare workers are commonly contaminated in the rooms of patients colonized or infected with MRSA or VRE. A number. |
|
Infection ou Colonisation: une source importante du mésusage
contamination : mise en évidence de microbes non présents dans le site prélevé • colonisation : présence de microbes sans infection associée |
|
De la colonisation à linfection - SPIADI
Colonisation de la portion intra-vasculaire ? favorisée par thrombus au niveau du KT De la colonisation à la contamination du cathéter |
|
Chaîne de transmission de linfection - INSPQ
transmission de microorganismes peut entraîner un portage passager une colonisation à long terme une infection asymptomatique ou une maladie clinique |
|
Colonisation versus Infection par le germe Pseudomonas aeruginosa
Colonisation versus Infection par le germe Pseudomonas aeruginosa M Carles Réanimation CHU Pointe-à-Pitre Abymes Faculté de Médecine Antilles-Guyane |
|
Influence de la colonisation à bactérie multirésistantes sur - DUMAS
18 déc 2015 · Les facteurs prédisposant d'infection nosocomiale sont soit liés à une augmentation du risque de colonisation soit à une diminution des |
|
Candidurie – colonisation ? Infection ? Quand et comment traiter ?
11 oct 2017 · contamination d'une colonisation ou d'une véritable infection locale ou disséminée justifiant un traitement antifongique |
|
Colonisation Et Infection À Acinetobacter Baumannii Dans Une
La colonisation cutanée joue un rôle important dans la contamination des mains du personnel et contribue à la dissémination de la bactérie au cours des |
|
PHYSIOPATHOLOGIE ET PRÉVENTION DES INFECTIONS SUR
La colonisation universelle n'est donc plus suffisante pour expliquer l'infection L'analyse de la diversité bactérienne a montré |
|
TRANSMISSION DES INFECTIONS DANS LES SERVICES DE
10 mar 2015 · abritent l'agent infectieux sans être infectés (colonisation) par exemple le SARM ? L'environnement (objets aliments sol air eau etc ); |
|
7 GEP colonisation bact - ORBi
La contamination se définit comme une présence passive du germe sans multiplica- tion La colonisation se caractérise par une mul- tiplication bactérienne qui |
Quelle est la différence entre la contamination et la colonisation ?
La contamination se définit comme une présence passive du germe sans multiplica- tion. La colonisation se caractérise par une mul- tiplication bactérienne qui dépasse les capacités locales de défense, mais sans toutefois induire des signes cliniques.Quels sont les modes de contamination ?
Modes de transmission des bactéries et des virus
Les piqures de moustiques, les morsures d'animaux, les seringues infectées sont des exemples plus concrets de ce mode de transmission. Les virus et les bactéries peuvent aussi se transmettre par la muqueuse respiratoire.C'est quoi une colonisation de l'arbre urinaire ?
Colonisation. L'arbre urinaire est normalement stérile à l'exception de la partie distale de l'urètre. Une colonisation correspond à la présence d'un (ou de plusieurs) micro-organisme dans l'arbre urinaire sans qu'il ne génère par lui- même de manifestations cliniques.- L'infection des bactéries par leurs virus se déroule en quatre étapes principales qui sont: (i) la reconnaissance spécifique de la cellule hôte et l'entrée du génome dans le cytoplasme, (ii) la réplication du génome viral, (iii) l'assemblage des particules virales, et (iv) leur rel?hement, menant dans la plupart des
Qu'est-ce qu'une colonisation urinaire ?
Comment se fait la colonisation de l'organisme ?
. Les chercheurs développent des moyens de contrer cette adhésion afin d'enrayer le processus infectieux.
Comment on attrape une septicémie ?
. Les infections urinaires , qui ne sont pas traitées à temps ou correctement peuvent induire une septicémie.
. Il arrive que des infections de l'abdomen et des plaies en soient également responsables .
|
Infection ou Colonisation - Infectiologie
contamination : mise en évidence de microbes non présents dans le site prélevé • colonisation : présence de microbes sans infection associée • infection |
|
CP04 - Par le germe Pseudomonas aeruginosa - SF2H
Colonisation versus Infection par le germe Passage de l'infection aigue à la colonisation/infection chronique ? Contamination d'origine ? 30-60 |
|
INFECTIONS URINAIRES COMMUNAUTAIRES
L'incidence des infections urinaires (IU) en France est estimée Une colonisation urinaire correspond à une contamination) et d'effectuer un antibiogramme |
|
INFECTIONS URINAIRES DE LADULTE ET DE LENFANT - CUEN
14 sept 2018 · crobiennes reflètent en général une contamination de l'ECBU) et que cette bactérie La colonisation urinaire n'est pas une infection urinaire |
|
Chaîne de transmission de linfection - INSPQ
COMITÉ SUR LES INFECTIONS NOSOCOMIALES DU QUÉBEC une colonisation à long terme, une sécrétions contaminées lors d'un éternuement ou la |
|
COLONISATION BACTERIENNE DU NOUVEAU-NE ET INFECTION
permettant la colonisation des surfaces épithéliales par which increase the risk of acquired neonatal infection contamination par des germes particulière- |
|
Infection urinaire - CPIAS Occitanie
Primordial +++ Techniques bactério étant très diverses Permet au labo de distinguer : • contamination par flore commensale • colonisation • infection réelle |
|
IAS entier2pptx [Lecture seule] - IFSI DIJON
1 Notion de Colonisation / infection • 2 Infections nosocomiales(IN) /Associées aux soins (IAS) • 3 peut dériver d'une contamination ou d'une inoculation |
|
Colonisation à bactéries multirésistantes en service de réanimation
Colonisation- infection nosocomiale Délai entre colonisation et infection La contamination des mains ou des gants s'effectue au contact du patient colonisé |