 Manuel de transmission du reporting PSF
Manuel de transmission du reporting PSF
La Bourse de Luxembourg met à disposition des entités ces feedbacks depuis le site www.e-file.lu. 1.1 Les circulaires CSSF de référence. Le reporting PSF : Pour
 Manuel de transmission du reporting bancaire
Manuel de transmission du reporting bancaire
Manuel de transmission du reporting bancaire. TAF MiFID. COREP. FINREP. Tableaux B2.3 B6.3 et B4.4. Enquêtes spécifiques de la CSSF. OTHER pour la CSSF.
 2022 NHSN Patient Safety Component Manual
2022 NHSN Patient Safety Component Manual
3 ian. 2022 Facilities that participate in certain reporting programs operated by the Centers for Medicare and Medicaid Services (CMS) can do so through use ...
 Manuel de transmission du reporting SICAR
Manuel de transmission du reporting SICAR
- Circulaire CSSF 08/344 du 12.03.2008 : Dispositions relatives à la transmission des fichiers de reporting à la CSSF. 1.2 Règle de nommage des rapports. Ceci
 Resource Guide on Good Practices in the Protection of Reporting
Resource Guide on Good Practices in the Protection of Reporting
34 https://www.bheuu.gov.my/portal/pdf/Akta/Act%20711.pdf. 35 Technical Guide to the United Nations Convention against Corruption page 105. Page 34. 24.
 FATCA XML Schema v2.0 User Guide (Draft 8-2016)
FATCA XML Schema v2.0 User Guide (Draft 8-2016)
Provides instructions on how to use the International Data Exchange Service to transmit FATCA reporting data. ? Publication 5188. FATCA Metadata XML Schema
 The Greenhouse Gas Protocol
The Greenhouse Gas Protocol
GHG Protocol Corporate Accounting and Reporting Standard (this document which electricity transmission and distribution losses.
 Guide to key performance indicators
Guide to key performance indicators
Narrative reporting - whether in the form of an Operating and. Financial Review (OFR) Management Discussion and Analysis. (MD&A)
 Data and Metadata Reporting and Presentation Handbook
Data and Metadata Reporting and Presentation Handbook
24 oct. 2006 into presentation in any detail and specify the provision of data to Eurostat through file transfer. Eurostat's manual on short-term ...
 Service déposant - prérequis
Service déposant - prérequis
MANUEL DE TRANSMISSION DES RAPPORTS B (Banque) P (PSF)
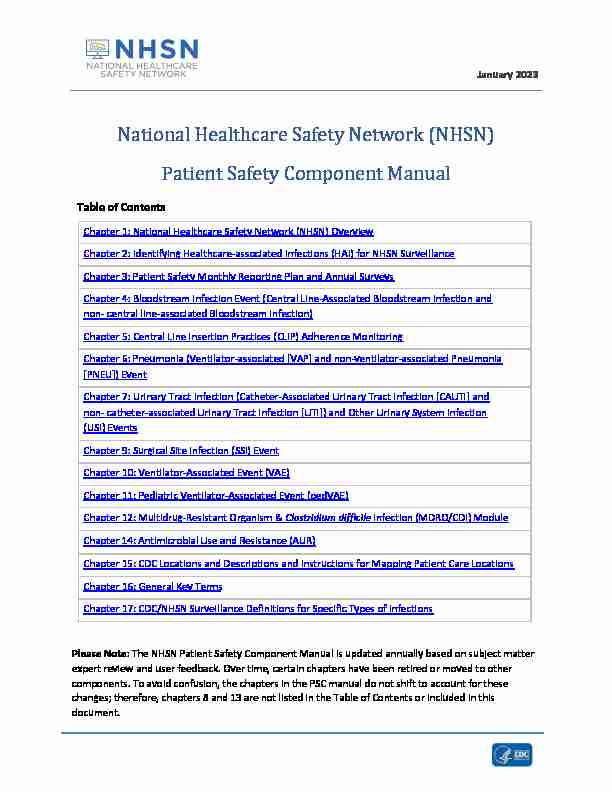 January 202ϯNational Healthcare Safety Network (NHSN)
January 202ϯNational Healthcare Safety Network (NHSN) Patient Safety Component Manual
Table of Contents
Chapter 1: National Healthcare Safety Network (NHSN) Overview Chapter 2: Identifying Healthcare-associated Infections (HAI) for NHSN Surveillance Chapter 3: Patient Safety Monthly Reporting Plan and Annual Surveys Chapter 4: Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and non- central line-associated Bloodstream Infection) Chapter 5: Central Line Insertion Practices (CLIP) Adherence Monitoring Chapter 6: Pneumonia (Ventilator-associated [VAP] and non-ventilator-associated Pneumonia [PNEU]) Event Chapter 7: Urinary Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and
non- catheter-associated Urinary Tract Infection [UTI]) and Other Urinary System Infection(USI) Events Chapter 9: Surgical Site Infection (SSI) Event Chapter 10: Ventilator-Associated Event (VAE) Chapter 11: Pediatric Ventilator-Associated Event (pedVAE) Chapter 12: Multidrug-Resistant Organism & Clostridium difficile Infection (MDRO/CDI) Module Chapter 14: Antimicrobial Use and Resistance (AUR) Chapter 15: CDC Locations and Descriptions and Instructions for Mapping Patient Care Locations
Chapter 16: General Key erms Chapter 17: CDC/NHSN Surveillance Definitions for Specific Types of Infections Please Note: The NHSN Patient Safety Component Manual is updated annually based on subject matter
expert review and user feedback. Over time, certain chapters have been retired or moved to other components. To avoid confusion, the chapters in the PSC manual do not shift to account for these changes; therefore, chapters 8 and 13 are not listed in the Table of Contents or included in this document.January 2023
1 - 1 National Healthcare Safety Network (NHSN) Overview
The NHSN is a secure, Internet-based surveillance system that expands and integrates patient and healthcare personnel safety surveillance systems managed by the Division of Healthcare Quality Promotion (DHQP) at the Centers for Disease Control and Prevention. F acilities that participate in certainreporting programs operated by the Centers for Medicare and Medicaid Services (CMS) can do so through
use of NHSN. Furthermore, some U.S. states use NHSN as a means for healthcare facilities to submit data on healthcare-associated infections (HAIs) and other healthcare measures mandated through their specific state legislation.NHSN enables healthcare facilities to collect and use data about HAIs, adherence to clinical practices
known to prevent HAIs, the incidence or prevalence of multidrug-resistant organisms within theirorganizations, trends and coverage of healthcare personnel safety and vaccination, and adverse events
related to the transfusion of blood and blood products.The NHSN includes
seven components: Patient Safety, Long-term Care Facility, Outpatient Dialysis, Healthcare Personnel Safety, Biovigilance, Outpatient Procedure, and Neonatal (Figure 1).Figure 1: NHSN Components
January 2023 NHSN Overview
1 - 2 The Patient Safety Component includes five modules that focus on events associated with medical devices, surgical procedures, antimicrobial agents used during healthcare, and multidrug resistant organisms.Device-associated Module:
o Bloodstream Infection (CLABSI - Central line-associated bloodstream infection) o Central line insertion practices (CLIP) adherence o Urinary Tract Infection (CAUTI - Catheter-associated urinary tract infection) o Pediatric Ventilator-associated events (PedVAE) (NICU and pediatric locations only) o Ventilator-associated events (VAE) (adult locations only) o Pneumonia (VAP - Ventilator-associated pneumonia) - in pediatric locations (in-plan* or off plan*), or NICU and adult locations (off-plan* only)Procedure-associated Module:
o Surgical Site Infection (SSI)Antimicrobial Use and Resistance Module (AUR)
Multidrug-Resistant Organism and Clostridium difficile Infection (MDRO/CDI) Module*Note: "In-plan" surveillance means that the facility has committed to following the NHSN surveillance
protocol, in its entirety, for that particular event, as shown in the facility'sNHSN monthly reporting plan.
"Off-plan" surveillance is surveillance that is done because a facility has decided to track a particular event
for internal use. Data that are entered into NHSN "off-plan" are not included in NSHN annual reports or
other NHSN publications. A facility makes no commitment to follow the NHSN protocol for "off-plan"events. Further, "off-plan" data cannot be uploaded into NHSN via Clinical Document Architecture (CDA)
and must be manually entered. Instructions and standardized surveillance methods and definitions for each module of the Patient Safety Component are provided in this manual and on the NHSN website (www.cdc.gov/nhsn). Modules may be used singly or simultaneously.The NHSN Long-term Care Facility Component provides long-term care facilities (LTCFs) with standardized
surveillance methods and definitions for four modules: (1) Multidrug resistant organism (MDRO) andClostridioides difficile Infection (CDI) laboratory-identified (LabID) Events; (2) Urinary Tract Infections
(UTI); (3) Prevention Process Measures; and 4) COVID-19. The component is ideal for use by nursinghomes, skilled nursing facilities, chronic care facilities, assisted living and residential care facilities,
intermediate care facilities for individuals with intellectual disabilities, psychiatric residential treatment
facilities, and State Veteran's Homes. LTCF surveillance protocols, training materials, data collection
forms, instructions, and other supporting materials are provided on the Long-term Care Facility Component website: https://www.cdc.gov/nhsn/ltc/index.html.Outpatient hemodialysis centers have several surveillance options tailored to their patients and setting in
the Dialysis Component. The component consists of 4 modules: 1) Dialysis Event; (2) Prevention Process
Measures; (3) Dialysis Patient Influenza Vaccination; and 4) COVID-19. Facilities that treat hemodialysis
outpatients should refer to the Dialysis Component instructions and standardized surveillance methods
and definitions at www.cdc.gov/nhsn/dialysis/index.html. There are two modules in the Healthcare Personnel Safety (HPS) Component of NHSN: The Healthcare Personnel Exposure Module and the Healthcare Personnel Vaccination Module. The HealthcareJanuary 2023 NHSN Overview
1 - 3Personnel Exposure Module
includes Blood/Body Fluid Exposure Only; Blood/Body Fluid Exposure with Exposure Management; and Influenza Exposure Management.This module is no longer available for
enrollment and should only be used by facilities that have already been reporting Blood/Body Fluid Exposure and Exposure Management data to the system.The Healthcare Personnel Vaccination Module
includes Influenza Vaccination Summary and COVID-19 Vaccination Summary. Data collected in thissurveillance system can assist healthcare facilities, health systems, and public health agencies to monitor
and report trends in blood/body fluid exposures, to characterize antiviral medication use for exposures to influenza, and to monitor influenza and COVID-19 vaccination coverage among healthcare personnel.These modu
les may be used separately or simultaneously. Instructions and standardized surveillance methods and definitions for the Healthcare Personnel Vaccination Summary is provided in the NHSNManual: HPS Component Protocol
vaccine-protocol.pdf . Information on reporting COVID-19 Vaccination Summary data for healthcare personnel can be found here: The NHSN Biovigilance Component, Hemovigilance Module facilitates national surveillance of transfusion-related recipient adverse events. The Hemovigilance Module is designed for transfusionservice staff to collect data on annual facility and transfusion service characteristics, individual reports on
adverse transfusion reactions, errors or accidents associated with adverse reactions, a nd monthly counts of transfused or discarded components. The Hemovigilance Module surveillance protocol, training materials, data collection forms, instructions, and other supporting materials are provided on theHemovigilance Module website:
www.cdc.gov/nhsn/acute -care-hospital/bio-hemo/index.html. The Outpatient Procedure Component (OPC) includes two modules that focus on adverse events associated with surgical procedures performed in Ambulatory Surgery Centers (ASCs). The two modules include Same Day Outcome Measures and Surgical Site Infections. Same Day Outcome Measures (OPC-SDOM) are a grouping of outpatient care quality indicators that represent a broad range of risks encountered by patients accessing care in various outpatient settings. The four individual outcome measures are: o Patient Burn o Patient Fall o Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant o All-Cause Hospital Transfer/Admission Surgical Site Infection (OPC-SSI) - SSI surveillance for outpatient operative procedures using theOutpatient Procedure Component (OPC).
The OPC surveillance protocols, training materials, data collection forms, instructions, and other supporting materials are provided on the Outpatient Procedure Component website: The Neonatal Component includes one module, Late-Onset Sepsis/ Meningitis (LOS/MEN). This modulewill track late-onset sepsis and meningitis events in very low birthweight neonates housed in Level II/III,
Level III, and Level IV nursery locations. The following events will be tracked in the LOS/MEN module:
January 2023 NHSN Overview
1 - 4 Late-Onset Sepsis Event: In an eligible infant, a recognized pathogen or common commensal identified from one or more blood specimens by a culture or non-culture based microbiologic testing method which is performed for purposes of clinical diagnosis or treatment. Under this major type of infection, there are two specific types of infection (see below). o NLCBI 1 o NLCBI 2 Meningitis Event: In an eligible infant, a recognized pathogen or common commensal identified from a CSF specimen by a culture or non-culture based microbiologic testing method which is performed for purposes of clinical diagnosis or treatment. Under this major type of infection, there are two specific types of infection (see below). o NLCM 1 o NLCM 2The LOS/MEN
surveillance protocols, training materials, data collection forms, instructions, and other supporting materials are provided on theNeonatal Component website:
Surveillance Techniques
Surveillance for healthcare acquired conditions/infections require a combination of active, concurrent,
prospective or retrospective approaches and surveillance techniques and resources. Trained InfectionPreventionists and designee
s shall seek out infections/conditions by screenin g a variety of data sources,such as laboratory, pharmacy, admission/discharge/transfer, radiology/imaging, and pathology databases,
as well as patient charts, including history and physical exam notes, nurses'/ physicians' notes, temperature charts, etc. Others may be trained to screen data sources for these events, but the IP mustmake the final determination. Laboratory-based surveillance should not be used alone, unless all possible
criteria for identifying an infection are solely determined by laboratory evidence (for example, LabID event detection in the MDRO/CDI Module). Retrospective chart reviews should be used only whenpatients are discharged before all information can be gathered. NHSN forms should be used to collect all
required data, using the NHSN definitions of each data field. To minimize the IP's data collection burden,
others may be trained to collect the denominator data and process of care data; additionally, electronic
capture of data is an option for reporting as an aide to optimizing available resources.Procedure-Associated Module
Surgical site infection (SSI) monitoring is offered through this module.SSI surveillance requires active,
patient- based, prospective surveillance techniques (see Surveillance Techniques above). To minimize IPs'workload of collecting denominator data, operating room data may be downloaded (see file specifications
at https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/ImportingProcedureData.pdf)SSI monitoring requires active, patient
based, prospective surveillance. Concurrent and post-discharge surveillance methods should be used to detect SSIs followin g inpatient operative procedures and post discharge surveillance for outpatient operative procedures.These methods may include 1) direct
examination of patients" wounds during hospitalization, or follow-up visits to either surgery clinics or
January 2023 NHSN Overview
1 - 5physicians" offices, 2) review of medical records or surgery clinic patient records, 3) visits to the ICU and
wards; talk with primary care staff 4 ) surgeon surveys by mail or telephone, and5) patient surveys by mail
or telephone (though patients may have a difficult time assessing their infections). Any combination of
these methods (or other methods identified by the facility) with the capacity to identify all SSIs is
acceptable for use; however, NHSN criteria for SSI must be used. See Surgical Site Infection Event (SSI)
protocol for additional examples of concurrent and post-discharge surveillance methodsDevice
-Associated Module Medical instrumentation increases the risk of development of an HAI and most patients admitted forhealth care are exposed to a medical device in the course of their treatment. Such devices include, but
are not limited to, vascular and urinary catheters, and ventilators. NHSN enables facilities to monitor infectious complications associated with the use of these devices an d to monitor processes related totheir use which might increase infection risk. Specifically, surveillance of central line-associated
bloodstream infection (CLABSI), catheter-associated urinary tract infection (CAUTI), ventilator-associated
events (VAE and PedVAE), and/or ventilator-associated pneumonia (VAP) is possible using the NHSN. In
addition, central line insertion practices (CLIP) can be monitored 'off plan' to inform facilities of the appropriateness of their processes and how they may relate to HAI development. See Dialysis Component for detailed instructions for Dialysis Event (DE) surveillance of hemodialysis outpatients (www.cdc.gov/nhsn/dialysis/index.html). Device-associated denominator data should be collected at the same time each day, or by weekly sampling methods in certain locations, for CLABSI, CAUTI, VAE, PedVAE, and VAP surveillance (see the CLABSI, CAUTI, VAE, PedVAE, and PNEU protocols for guidance). When denominator data are availablefrom electronic databases (for example, ventilator days from respiratory therapy), these sources may be
used as long as the counts are not substantially different (+/- 5%) from manually-collected counts that
have been validated for a minimum of three months. See the respective device-associated event protocols for detailed surveillance instructions.Antimicrobial Use and Resistance (AUR) Module
The use of antimicrobial agents has a direct effect on antimicrobial resistance patterns of pathogens. The
observed increase in multidrug resistance is in part due to inappropriate prescription of, as well as
only partial completion of courses of antibiotics. The AUR Module allows facilities to collect information on the amount of anti microbials that are used forpatient care within their systems, as well as to collect data on the prevalence of drug-resistant organisms
in their inpatient and outpatient areas. Electronic capture and reporting of microbiology and pharmacy
data are the only available options for reporting data into this module. See the Antimicrobial Use and Resistance protocol for detailed surveillance instructions.January 2023 NHSN Overview
1 - 6 Multidrug-resistant Organism and Clostridium difficile Infection (MDRO/CDI)Module
The NHSN MDRO/CDI Module offers a means for facilities to meet criteria and metrics that are outlined in
several organizational guidelines to control and measure the spread of MDROs and CDI within their h ealthcare system. The module has two separate and independent reporting options, Laboratory- identified (LabID) Event and Infection Surveillance that may be tailored to meet the needs of participatingNHSN facilities.
In addition, the following process measures are available: (1) adherence to hand hygiene; (2) adherence
to contact precautions when caring for patients infected or colonized with an MDRO orC. difficile; and (3)
adherence to active surveillance testing (AST) of MRSA and/or VRE. Active surveillance testing outcome
measures is also available in locations where AST adherence is being performed and enables facilities to
use the results of AST to monitor the incidence and prevalence of positiveMRSA and/or VRE
cultures. See the MDRO/CDI protocol for detailed surveillance instructions.January 2023
2-1Identifying Healthcare
-associated Infections (HAI) for NHSNSurveillance
The purpose of Chapter 2 is to
standardize the classification of an infection as present on admission (POA)or a healthcare-associated infection (HAI), using objective surveillance definitions and guidance for NHSN
surveillance . The intention of this chapter is to align criteria and de finitions and decrease subjectivitywhile maintaining epidemiologic standardization and clinical relevance. A variety of scenarios to include
repeat infections of the same type, concurrent infections of differing types, and pathogen assignment in
multi-pathogen infections are addressed. See Appendix Flow Diagram for NHSN Event Determination.Table of
Contents General Instructions ........................................................................
............................................................. 1Infection Window Period (IWP) .................................................................................................................... 3
Infection Window Period Special Considerations ........................................................................................ 4
Date of Event (Event Date) ........................................................................................................................... 7
Location of Attribution (LOA) ................................................................................................
9Transfer Rule (Exception to Location of Attribution) ................................................................................... 9
Repeat Infection Timeframe (RIT) .............................................................................................................. 11
Secondary BSI Attribution Period
(SBAP) ................................................................................................... 14
Secondary BSI Attribution Period Tables: ................................................................................................... 16
Pathogen Assignment Guidance ................................................................................................................. 18
Appendix: Flow Diagram for NHSN Event Determination .......................................................................... 28General Instructions
1. The guidance found in this Chapter is not applicable when performing surgical site infection (SSI),
ventilator associated event (VAE), pediatric ventilator associated event (PedVAE) or laboratory- identified (LabID) event. Infection window period (IWP), date of event (DOE), present on admission (POA), healthcare-associated infection (HAI), and repeat infection timeframe (RIT), secondary BSI attribution period (SBAP) definitions as defined in this chapter do not apply to SSI,VAE, PedVAE, or LabID events (Table 1).
Refer to Chapters 9, 10, 11 and 12 for guidance specific to these event determinations. January 2023 Identifying Healthcare-associated Infections 2-2 Table 1: Module Exceptions to application of Chapter 2 Timeframes (Page 2-2)Concept SSI LabID VAE PedVAE
Infection Window Period
Not Applicable
Not Applicable
Not Applicable
Not Applicable
Date of Event
Present on Admission
Healthcare-associated Infection
Repeat Infection Timeframe
Secondary BSI Attribution Period
2. Organisms belonging to the following genera are typically causes of community-associated
infections and are rarely or are not known to be causes of healthcare-associated infections. They are excluded and cannot be used to meet any NHSN definition:Blastomyces, Histoplasma,
quotesdbs_dbs32.pdfusesText_38[PDF] ANNEXE : PROCEDURE DE SUIVI DES TEMPS VIA TEMPO
[PDF] Questions / Re ponses. Appel d offres relatif a la «Fiabilisation de l utilisation actuarielle d un entrepo t de donne es»
[PDF] Termes de références : AUDIT FINANCIER ET ORGANISATIONNEL DE LA COMMUNE URBAINE DE MAHAJANGA
[PDF] SCHEDULER NOTE. De nouvelles données, mieux exploitables Définition. Accès dans Engine
[PDF] Le point de vue du superviseur
[PDF] USAIN BOLT. Table des matières. Tâche complexe produite par l académie de Clermont-Ferrand. Juin 2012. Fiche professeur... 2. Fiche élève 1...
[PDF] EPCCI ÉCOLE PRATIQUE DE LA CHAMBRE DE COMMERCE & D INDUSTRIE DE CÔTE D IVOIRE NOTRE OFFRE DE FORMATION
[PDF] GUIDE D UTILISATION NOVEMBRE 2015
[PDF] Participaient à la séance : Olivier CHALLAN BELVAL, Hélène GASSIN, Jean-Pierre SOTURA et Michel THIOLLIERE, commissaires.
[PDF] Le péage urbain à Montréal
[PDF] Présentation des missions réalisées
[PDF] L assurance-accidents des chômeurs de A à Z. Couverture d assurance de la Suva 7 jours sur 7 et 24 heures sur 24
[PDF] JANVIER 2013 LIVRET D INFORMATION CARTES SO MUSIC. particuliers.societegenerale.fr
[PDF] RAPPORT DE SITUATION SUR LA SÉCURITÉ ROUTIÈRE DANS LE MONDE 2013
