 Use of Local Anesthesia for Pediatric Dental Patients
Use of Local Anesthesia for Pediatric Dental Patients
26 The effect of adjusting the pH of local anesthetics with epinephrine in dentistry is of interest as a way to reduce pain and time to onset of anesthesia.
 Comparison of buffered and non‑buffered lidocaine: pH and pain
Comparison of buffered and non‑buffered lidocaine: pH and pain
16 Sept 2022 Stewart JH Cole GW and Klein JA: Neutralized lidocaine with epinephrine for local anesthesia. J Dermatol Surg Oncol 15: 1081‑1088
 DATA SHEET
DATA SHEET
with pH 4.0-6.5. Page 2. MARCAIN ± Adrenaline Data Generally the dose of local anaesthetic solutions containing adrenaline equals that of plain solutions.
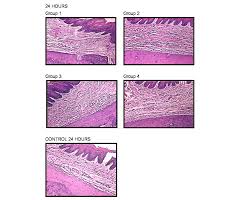 The influence of local anesthetic solutions storage on tissue
The influence of local anesthetic solutions storage on tissue
This increased inflammatory reaction could be attributed to the pH of the LAS studied. The pH of commercial LAS added with sympathomi- metic amines (epinephrine
 XYLOCAINE® 2%
XYLOCAINE® 2%
Adequate precautions should be taken to avoid prolonged contact between local anaesthetic solutions containing adrenaline (epinephrine) (low pH) and metal
 Xylocaine 1% Solution for Injection
Xylocaine 1% Solution for Injection
the local anaesthetic and the duration of exposure of the tissue to the local anaesthetic. solutions containing adrenaline (low pH) and metal surfaces (e.g. ...
 Buffered local anesthetics reduce injection pain and provide
Buffered local anesthetics reduce injection pain and provide
The pH of lidocaine (without epinephrine) in preparations used for local anesthesia varies between 3.5 and 7.0 (Cepeda et al. 2010)
 pHâ•adjustment and discomfort caused by the intradermal injection
pHâ•adjustment and discomfort caused by the intradermal injection
local anaesthesia with I % lignocaine I % lignocaine with adrenaline or the corresponding pH-adjusted solutions. The local anaesthetic solutions were.
 Stability of Adrenalin in Dental Local Anesthetics on the Different
Stability of Adrenalin in Dental Local Anesthetics on the Different
The re- sults suggest that the racemization reaction may prove to be an important route for loss of biological activity of adrenaline at pH values much below pH
 Efficacy of Sodium Bicarbonate Addition into Local Anesthetic
Efficacy of Sodium Bicarbonate Addition into Local Anesthetic
24 Oct 2022 Neutralized lidocaine with epinephrine for local anesthesia ... Randomised control trial of pH buffered lignocaine with adrenaline in outpatient ...
 Alkalinisation of local anaesthetic solutions
Alkalinisation of local anaesthetic solutions
Local anaesthetics are basic drugs which have a pKa (derived at a lower pH than the same solution without adrenaline ('plain solution').
 Comparison of buffered and non?buffered lidocaine: pH and pain
Comparison of buffered and non?buffered lidocaine: pH and pain
16 sept. 2022 Commonly used local anaesthetic (LA) solutions ... the pH of commercially available lidocaine with epinephrine. (pH 3.3?5.5) is lower than ...
 Buffered local anesthetics reduce injection pain and provide
Buffered local anesthetics reduce injection pain and provide
The pH of lidocaine (without epinephrine) in preparations used for local anesthesia varies between 3.5 and 7.0 (Cepeda et al. 2010)
 Use of Local Anesthesia for Pediatric Dental Patients
Use of Local Anesthesia for Pediatric Dental Patients
19 avr. 2007 the myocardium is sensitized to epinephrine and such ... The effect of adjusting the pH of local anesthetics in dentistry.
 Recommendations to use vasoconstrictors in dentistry and Oral
Recommendations to use vasoconstrictors in dentistry and Oral
local anaesthetic with adrenaline in the event of other with a pH of 68
 DATA SHEET
DATA SHEET
31 mai 2018 The pH of the solution is 3.3-5.0. ... of 3-5 mL short-acting local anaesthetic containing adrenaline is recommended. An.
 Effects of adrenaline and hyaluronidase on plasma concentrations
Effects of adrenaline and hyaluronidase on plasma concentrations
with adrenaline (5 ?g ml91); (III) local anaesthetic with hyaluronidase (75 iu ml91); or (IV) local (100 ?l) was added to adjust the samples to pH 11.
 JMCJMS
JMCJMS
adrenaline Sodium bicarbonate
 Local anaesthetic agent toxicity
Local anaesthetic agent toxicity
Refresher Course: Local anaesthesia agent toxicity. 2010;16(1). S Afr J Anaesthesiol Analg The clinical implication of this is that a decrease in pH.
 XYLOCAINE® 2%
XYLOCAINE® 2%
Adequate precautions should be taken to avoid prolonged contact between local anaesthetic solutions containing adrenaline (epinephrine) (low pH) and metal
 Local Anesthesia in Dentistry - SlideShare
Local Anesthesia in Dentistry - SlideShare
stability of adrenaline – the adrenaline added to some local anaesthetic solutions is unstable at the physiological pH and more stable at an acidic pH Commercially available acidic local anaesthetic solutions have a pH of typically 3 5 to 5 5 and have a shelf-life of three to four years
 Local anaesthetics in dentistry - Part 3 - SciELO
Local anaesthetics in dentistry - Part 3 - SciELO
Use of adrenaline should be deferred for patients who have suffered a cerebrovascular accident or stroke within the last six months After that time doses of adrenaline should be limited to less than 0 036 mg equivalent to two cartridges of local anaesthetic with 1:100000 adrenaline concentration 1617 HYPERTHYROIDISM
 Local anesthesia - Tishk International University
Local anesthesia - Tishk International University
Anesthesia literally means “no sensation” Derived from the Greek verb for “to perceive” Local anaesthetics (LAs) are the drugs that when applied topically or injected locally block nerve conduction and cause reversible loss of all sensation in the part supplied by the nerve
 Searches related to ph of local anesthesia with adrenaline filetype:pdf
Searches related to ph of local anesthesia with adrenaline filetype:pdf
Methodsof local anesthetic chemical formulations: (1) esters (eg procaine This revision included a new systematic literature searchbenzocaine of the tetracaine); and (2) amides (eg lidocaine- mepivaMEDLINE/Pubmed electronic database using the followingcaine prilocaine articaine)
What is the pH of local anesthetic?
- Based on tissue pH and anesthetic Pka . • Injectable local anesthetics are weak bases (pka=77.5-9.5) When a local anesthetic is injected into tissue it is neutralized and part of the ionized form is converted to non-ionized The non-ionized base is what diffuses into the nerve. 33
What is the concentration of adrenaline in local anaesthetics?
- Adrenaline can be used at concentration range from 1: 2 lakh to 1: 0.5 lakh; however, 1: 1 lakh concentration is often favoured for use. The enzyme hydrolyses ground substance (i.e. hyaluronic acid) so increases area of diffusion and hence area of effect of local anaesthetics.
Are local anaesthetics ionised at physiological pH?
- Most local anaesthetics are weak bases, with a pKa between 8 and 9, so that they are mainly but not completely ionised at physiological pH.your comments I agree with Dr Green, Dr V. Dinic and B. Smith. Tissue Acidosis (pH ~ 3-4,) caused a more ionised form, not permeable to the Cell membrane.
What is alkalinization in local anesthesia?
- BACKGROUND: Alkalinization, or buffering of local anesthesia, is a well-documented technique to mitigate low pH levels of the preparations with reports indicating clinical benefits such as decreased onset time and injection pain.
C o MM uni C ation I
NTRODUCTION
Vasoconstrictors like adrenaline in local anaesthetics are associated with more drug interactions than any other drug in Dentistry 1 with an incidence of adverse reactions ranging from 2.5%-11%. 2Therefore, understanding the
physiological and pharmacological effects, interactions with other drugs, and dosages are important in day to day dental practice. Local anaesthetics are vasodilators, hence the addition of a vasoconstrictor like adrenaline provides the following advantages: improves the anaesthetic onset and duration, reduces bleeding, and decreases the systemic absorption rate of local anaesthetics by reducing the plasma concentration.2,3However, adrenaline is unstable and
therefore an antioxidant is added to prevent it oxidizing. Sodium bisulphite is the preservative most commonly added to local anaesthetics. Of course, patients allergic to sulphites will now react to a local anaesthetic containing sodium bisulphites.DOSAGE
Calculating the dose of vasoconstrictor is different from ascertaining the local anaesthetic dosage in that vasoconstrictors are expressed as a dilution ratio and are not weight-dependent. In local anaesthetics, the adrenaline in dilution ratios of 1:80000 (Xylotox E80A, Adcock Ingram; Xylestesin, 3M), 1:100 000 (Ubistesin forte, 3M; Septocaine, Septodont) and 1:200000 (Ubistesin 3M; Septocaine, Septodont) are generally the most commonly used concentrations in dentistry. Adrenaline concentrations are generally expressed as1:1000 which is 1mg/ml. Therefore, a local anaesthetic
with 1:100000 adrenaline concentration will translate to0.01mg/ml resulting in a 1.8ml local anaesthetic cartridge
containing 0.018mg adrenaline. A 1:200000 will therefore contain a concentration of 0.005mg/ml translating to approximately 0.01mg per cartridge of local anaesthetic. The maximum dose of adrenaline in healthy patients is0.2mg per appointment (approximately 10 cartridges
of 1:100000 local anaesthetic). However, in medically compromised patients, such as those having cardiac risk,
the recommended maximum dosage of adrenaline is 0.04 mg i.e. two cartridges of 1:1000000 local anaesthetic. The American Heart Association and the American Dental Association have stated "the typical concentrations of vasoconstrictors contained in local anaesthetics are not contraindicated in cardiovascular disease so long as preliminary aspiration is practiced, the agent is injected slowly, and the smallest effective dose is administered".4 Adrenaline 1:100,000 caused more sympathomimetic side effects than did 1:200,000 adrenaline concentration 5 thus it is logical to use this lower concentration of adrenaline when possible. In several European and Asian countries, adrenaline concentrations of 1:300000 and 1:400000 are now available in dental cartridges. 6Furthermore, using
a lower concentration of adrenaline like 1:200000 does not seem to compromise the anaesthetic efficacy of the local anaesthetic. 7-9In fact, 1:200000 solutions should be
the preferred choice of adrenaline concentration in the absence of significant differences in performance with the1:100000 solution.10
For patients undergoing periodontal
surgery, 4% articaine with either adrenaline 1:100000 or1:200000 concentration provides excellent surgical pain
control. However, the 4% articaine 1:100000 adrenaline concentration has the additional advantage of providing better visualization of the surgical field because there is less bleeding. 11ADRENALINE AND DRUG INTERACTION
Another problem associated with adrenaline is that it can interact with some of the drugs that the patient may be taking. In this instance the most commonly affected drugs are the non-selective beta blockers, some antidepressants and "street drugs" (Table 1).NON-SELECTIvE BETA BLOCKERS Non-selective beta blockers like propranolol (Inderal) and nadolol (Corgard) are used as anti-hypertensive drugs or to control migraines. Vasoconstrictors administered to patients on non-selective beta blockers can result in uncompensated peripheral vasoconstriction as a result of unopposed stimulation of alpha 1 receptors, leading to increase in blood pressure, bradycardia and headaches.4,12,13 Cases have been recorded in both the dental and medical literature where the magnitude of the blood pressure saDJ May 2017, Vol 72 no 4 p176 - p178
D sMoodley
Local anaesthetics in dentistry - Part 3:
Vasoconstrictors in local anaesthetics
D s Moodley: PhD, MSc, PDD Aesthet. BDS, FICD. department of r estorative dentistry, Faculty of dentistry, university of the western Cape, Cape town, south africa. Private bag X1, tygerberg, 7505. tel: 021 9373090 e-mail: dmoodley@uwc.ac.za 177www.sada.co.za / sadJ vol 72 no. 4 C o MM uni C ation increased was alarming and potentially life threatening. 13 Therefore, in patients on non-selective beta blockers requiring simple restorative procedures, complete avoidance of adrenaline seems rational. For more complex procedures for which haemostasis or a more prolonged duration of local anaesthesia is required, the initial vasoconstrictor dose should be kept to an absolute minimum such as one-half of a dental cartridge with
1:100000 or preferably 1:200000 and injected carefully to
avoid intravascular administration. The vital signs of the patient should be monitored before further administration. If there is no change in cardiovascular status, additional cartridges can be injected individually at five-minute intervals. Adrenaline containing retraction cord must be avoided in a patient taking a non- selectiveȕ-antagonist.
TRICYCLIC ANTIDEPRESSANTS
Tricyclic antidepressants like imipramine and amitriptyline inhibit the uptake of adrenaline at the neuronal level, resulting in increased concentrations of the catecholamines at the sympathetic neuronal junction. 14A maximum dose of 0.04 mg,
(equivalent to two cartridges of 1;100000 local anaesthetic) of exogenous adrenaline is proposed for patients on tricyclic antidepressants. 15Using a lower concentration of 1:100000or
less, eg. 1:200000, is preferable and in a dosage which is no more than one-third the normal maximum which would be given, should preclude any problem that could arise from a tricyclic drug interaction. 1 The interactions of vasoconstrictors with general anaesthet- ics like halothane, thiopental and barbiturates can increase the dysrhythmic effects of dental vasoconstrictors. The cli- nician needs to inform the anaesthetist before administer- ing a local anaesthetic with vasoconstrictor, and to restrict the dose to the limit recommended for the vasoconstrictor according to general anaesthetic procedures: halothane (2.2µgkg for halothane, 3.5µg/kg for enflurane and 5.5µg/ kg for isoflurane). 1,15A reported death under halothane an-
aesthesia caused by adrenaline in gingival retraction cord reinforces the need to adhere to recommended doses of adrenaline under general anaesthesia. "STREET DRUGS" Methamphetamines and cocaine have sympathomimetic effects and can interact with adrenaline in local anaesthetics. Vasoconstrictors in combination with cocaine or methamphetamines increase the risk of hypertensive crises, stroke and myocardial infarction. 4Elective dental
treatment should be postponed for at least 24 hours after the last cocaine use to allow elimination of the drug. 3ADRENALINE AND THE MEDICALLY
COMPLEx PATIENT
Adrenaline is both a hormone and a neurotransmitter belonging to sympathomimetic drugs that can mimic sympathetic nervous system mediators. 6It provides direct
stimulation of the adrenergic receptors. Clinicians need to be aware of its effect on the sympathetic nervous system especially in medically compromised patients as certain modifications must be made (Table 1). A joint statement of the American Dental Association and American Heart Foundation on vasoconstrictors provides the following advice: "Vasoconstrictors should be used with extreme care to avoid intravascular injection. The minimum possible amount of vasoconstrictor should be used". 6CARDIOvASCULAR DISEASES
In the presence of ischaemic heart disease, elective dental treatment is contraindicated in the following situations: patients with unstable angina, recent myocardial infarction (less than six months), recent coronary artery bypass surgery (less than three months). 16 If emergency dental treatment is necessary, medical consultation is required and adrenaline dosages should be limited to one to two cartridges of 1:100000 solution (0.018 to 0.036 mg of adrenaline). 16,17Similarly, in patients with
stable angina, vasoconstrictors should be limited to one to two cartridges. 16Vasoconstrictors are contraindicated
in patients with severe arrhythmias. 10Digoxin, prescribed
to increase the heart's contractile force, has a narrow therapeutic index and may precipitate a cardiac arrhythmia when used concurrently with vasoconstrictors. 16,17STROKE
Use of adrenaline should be deferred for patients who have suffered a cerebrovascular accident, or stroke within the last six months. After that time, doses of adrenaline should be limited to less than 0.036 mg, equivalent to two cartridges of local anaesthetic with 1:100000 adrenaline concentration. 16,17HYPERTHYROIDISM
The use of adrenaline in local anaesthetics should be avoided, or at least minimized to one to two cartridges, in the untreated or poorly controlled hyperthyroid patient. 18 Although the theoretical risk of thyroxine - adrenaline potentiation is serious, no clinical case has been reported. 10Table 1:
Precautions regarding adrenaline usage in local anaesthetics.Contraindications to vasoconstrictors in dentistryPrecautions to the use of vasoconstrictors in dentistry
Heart diseases:
Unstable angina, Recent myocardial infarction, Recent coronary artery bypass surgery, Refractory arrhythmias, Untreated or uncontrolled congestive heart failure.Untreated or uncontrolled severe hypertension,
Uncontrolled hyperthyroidism
Uncontrolled diabetes
Sulphite allergies
Steroid-dependent asthma
Pheochromocytoma
Patients taking tricyclic antidepressants
Patients taking phenothiazine compounds
Patients taking monoamine oxidase inhibitors
Patients taking nonselective Beta-blockers
Cocaine abusers
Patients undergoing general anaesthesia with HalothanePatients taking Digoxin
178C o MM uni C ation
CORTICOSTEROID-DEPENDENT ASTHMA
Administration of local anaesthetic with vasoconstrictors in cortico-dependent asthma patients may result in a higher risk of sulphite allergy. An anaesthetic without vasoconstrictor, and thus without bisulphite, is indicated.4,10,17
PHEOCHROMOCYTOMA
A tumour of the adrenaline medulla, characterized by the presence of catecholamine-producing tissue, constitutes an absolute contraindication to the administration of vasoconstrictors. 10BONE IRRADIATION
It is desirable to avoid the use vasoconstrictors with a local anaesthetic when a patient is receiving irradiation of bone. 10 CONCLUSION
A thorough understanding of the pharmacologic interactions between adrenaline and vasoconstrictors is important to avoid untoward reactions in patients. A lower concentration like 1:200000 provides similar vasoconstriction and may be preferred especially for medically compromised patient.References
Yagiela JA. Adverse drug interactions in dental practice: 1. interactions associated with vasoconstrictors. Part V of a series. J Am Dent Assoc. 1999;130(5):701-9. Kaufman E, Garfunkel A, Findler M, Elad S, Zusman SP, 2. Malamed SF, et al. Emergencies evolving from local anesthesia. Refu'at hapeh veha-shinayim. 2002 Jan;19(1):13-8, 98. Balakrishnan R, Ebenezer V. Contraindications of 3. vasoconstrictors in Dentistry. Vol. 6, Biomedical andPharmacology Journal. 2013. p. 409-14.
Bassett K, DiMarco A, Naughton D. Local Anesthesia for 4. Dental Professionals. 2nd ed. DiMarco Arthur NDBK, editor.New Jersey: Pearson Education Inc; 2015. 1-418 p.
complications associated with local anesthesia in dentistry.Anesth Prog. 1997;44(4):132-41.
Malamed SF. Handbook of Local Anesthesia. 6th ed. Malamed 6. SF, editor. Vol. 33, Elsevier. St. Louis: Elsevier Mosby; 2013.25-38 p.
Mcentire M, Nusstein J, Drum M, Reader A, Beck M. 7. Anesthetic efficacy of 4% articaine with 1:100,000 epinephrine versus 4% articaine with 1:200,000 epinephrine as a primary buccal infiltration in the mandibular first molar. J Endod.2011;37(4):450-4.
Santos CF, Modena KCS, Giglio FPM, Sakai VT, Calvo AM, 8. Colombini BL, et al. Epinephrine concentration (1:100,000 or1:200,000) does not affect the clinical efficacy of 4% articaine
for lower third molar removal: a double-blind, randomized, crossover study. J Oral Maxillofac Surg. 2007; Wahl MJ, Ilvento TW, Schmitt MM, Wahl JA, Ganjavian S. 9. Articaine with 1:100000 epinephrine versus articaine 1;200000 epinephrine. e-Journal Dent. 2013;3(2):371-5. Carlos M, Bruno C, Ronneau M. Recommendations to use 10. vasoconstrictors in Dentistry and Oral Surgery. Médecine buccale Chir buccale. 2003;9(2):1-30. Moore P, Doll B, Delie R, Hersh E, Korostoff J, Johnson S, 11. et al. Hemostatic and anesthetic efficacy of 4% articaine HCl with 1:200,000 epinephrine and 4% articaine HCl with1:100,000 epinephrine when administered intraorally for
periodontal surgery. J Periodontol. 2007;78(2):247-53. Hersh E V, Moore PA. Three serious drug interactions that 12.every dentist should know about. Compend Contin Educ Dent. 2015;36(6):408-13. Hersh E V, Giannakopoulos H. Beta-adrenergic blocking 13.
agents and dental vasoconstrictors. Dent Clin North Am.2010;54(4):687-96.
Sisk AL. Vasoconstrictors in local anesthesia for Dentistry. 14.Anesth Prog. 1992;39:187-93.
Gómez-Moreno G, Guardia J, Cutando A, Calvo-Guirado JL. 15. Pharmacological interactions of vasoconstrictors. Med Oral Patol Oral Cir Bucal Med Oral Patol Oral Cir Bucal Jan MedOral S L CIF B. 2009;141414(11):20-7.
Domingo D, Canaan T. Local anesthetics (Part III): use in 16. medically complex patients. Clin Updat. 2002;24(11):22-4. Budenz AW. Local anesthetics and medically complex 17. patients. J Calif Dent Assoc. 2000;28:611-9. Perusse R, Goulet JP, Turcotte JY. Contraindications to 18. vasoconstrictors in Dentistry: Part II. Hyperthyroidism, diabetes, sulphite sensitivity, cortico-dependent asthma, and pheochromocytoma. Oral Surgery, Oral Med Oral Pathol.1992;74(5):687-91.
quotesdbs_dbs20.pdfusesText_26[PDF] phaeacians in the odyssey
[PDF] phagocytosed food is digested in
[PDF] phagocytosed meaning in urdu
[PDF] phagocytosed particle
[PDF] phagocytosed synonym
[PDF] pharma braille
[PDF] pharmaceutical analysis 1 pdf
[PDF] pharmaceutical application of artificial intelligence
[PDF] pharmaceutical cosmetics books pdf
[PDF] pharmacist drug information resources
[PDF] pharmacodynamie pharmacocinétique
[PDF] pharmacologie cours
[PDF] pharmacologie pdf
[PDF] pharmacologue définition simple
