[PDF] crise hypertensive conduite a tenir
[PDF] pic hypertensif
[PDF] reduire son apport calorique pour maigrir
[PDF] diminuer les quantités pour perdre du poids
[PDF] reduire les calories et le tour de taille en 14 et
[PDF] regime pour maigrir pdf
[PDF] que représente 2000 calories par jour
[PDF] réduire apport calorique
[PDF] calorimétrie formule
[PDF] calorimétrie tp corrigé
[PDF] calorimétrie tp chimie
[PDF] calorimétrie définition
[PDF] exercice calorimétrie bts
[PDF] diplome anglais international
Oxtober 20101Confidential
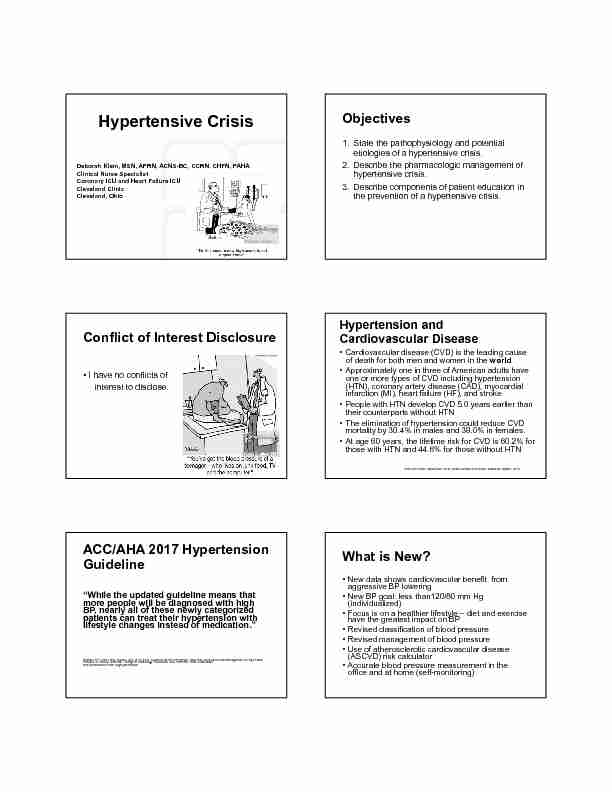
Hypertensive Crisis
Deborah Klein, MSN, APRN, ACNS-BC, CCRN, CHFN, FAHAClinical Nurse Specialist
Coronary ICU and Heart Failure ICU
Cleveland Clinic
Cleveland, OhioObjectives
1. State the pathophysiology and potential
etiologies of a hypertensive crisis.2. Describe the pharmacologic management of
hypertensive crisis.3. Describe components of patient education in
the prevention of a hypertensive crisis.Conflict of Interest Disclosure • I have no conflicts of interest to disclose.Hypertension and
Cardiovascular Disease
• Cardiovascular disease (CVD) is the leading cause of death for both men and women in the world
• Approximately one in three of American adults have one or more types of CVD including hypertension (HTN), coronary artery disease (CAD), myocardial infarction (MI), heart failure (HF), and stroke
• People with HTN develop CVD 5.0 years earlier than their counterparts without HTN • The elimination of hypertension could reduce CVD mortality by 30.4% in males and 38.0% in females. • At age 60 years, the lifetime risk for CVD is 60.2% forthose with HTN and 44.6% for those without HTNAmerican Heart Association. 2018 Heart Disease and Stroke Statistical Update, 2018.
ACC/AHA 2017 Hypertension
Guideline"While the updated guideline means that
more people will be diagnosed with highBP, nearly all of these newly categorized
patients can treat their hypertension with lifestyle changes instead of medication."Whelton PK, Carey RM, Aronow WS, et al. 2017 Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. American College of Cardiology Foundation and American Heart Association.
http://professional.heart.org/hypertension.• New data shows cardiovascular benefit from aggressive BP lowering • New BP goal: less than120/80 mm Hg (individualized) • Focus is on a healthier lifestyle - diet and exercise have the greatest impact on BP • Revised classification of blood pressure • Revised management of blood pressure • Use of atherosclerotic cardiovascular disease (ASCVD) risk calculator • Accurate blood pressure measurement in the office and at home (self-monitoring) What is New?2017 Classification of Blood
Pressure
Blood Pressure
CategorySystolic Diastolic (mm Hg) (mm Hg)Normal Less than andless than 80
120Elevated 120-129 andless than 80
Hypertension
Stage 1 130-139 or80-89
Hypertension
Stage 2 140 or 90 or higher
or higherEssential (Primary) Hypertension
• "Silent killer" as it usually has no symptoms • Most common risk factor for MI and stroke • 34% of American adults have HTN • Of these with HTN, about 76% are using anti- hypertensive medications, but only 54.4% have their condition controlled • 90-95% of cases of HTN have no known cause, but risk factors have been identified American Heart Association. 2018 Heart Disease and Stroke Statistical Update, 2018.Nonmodifiable Risk Factors
•Race African Americans develop HTN more often, earlier, and more severe than Caucasians •Family history The risk of HTN increases if parents, brothers, sisters, or children have the disease. •AgeThe risk of HTN increases with age. A higher percentage of men have HTN until age 45. From age 45-60, the percentage of men and women are similar. After age 60, a higher percentage of women have HTN.
American Heart Association. 2018 Heart Disease and Stroke Statistical Update, 2018Modifiable Risk Factors
•ObesityBMI 30 are more likely to develop HTN
•High-sodium diet Excess sodium intake (e.g. >3000 mg/day) increases risk for HTN •Lack of physical activity Inactive lifestyle promotes weight gain and increases for HTN •Stress/hostile attitudes/impatience •Dyslipidemia and diabetes •Excessive alcohol consumption American Heart Association. 2018 Heart Disease and Stroke Statistical Update, 2018Pathophysiology of HTN
• Poorly understood but a variety of factors have been implicated • Increased sympathetic nervous system activity •Ĺ HR •Ĺ peripheral resistance (vasoconstriction) • Vascular remodeling with narrowing and vasospasm of arteries •Ĺ insulin resistance contributing to endothelial dysfunction and Ļ production of vasodilators • Increased renin-angiotensin-aldosterone activity • Sodium and water retention • Vasoconstriction • Hypertrophy of myocardium associated with HTN • GeneticsHTN and CAD
• HTN causes microscopic tears in the artery walls that then turn into scar tissue • Scar tissue provides a place for plaque to develop • Arteries slowly harden and narrow resulting in peripheral artery disease (PAD) and CAD • As one ages, arteries harden and become less elastic • Ongoing HTN accelerates this process • Blood flow impaired to major organs leading to risk of blood clots, CAD, stroke, and renal damageHTN Complications
• Left ventricular hypertrophy with Ĺrisk for heart failure, ventricular arrhythmias, MI, and death
• Most common and important risk factor for the development of stroke and intracerebralhemorrhage
• Chronic and end-stage kidney disease • Retinopathy •Marked elevations in BP can cause acute,life-threatening emergenciesDefinitions
•Resistant HTN: BP greater than goal despite the concurrent use of 3 antihypertensive agents of different classes, including a diuretic
•Hypertensive urgency: acute increase in BP in the absence of symptoms suggesting acute organ damage
•Hypertensive emergency: acute increase in BP associated with severe, potentially life-threatening target organ damage
• "Acute increase in BP": • systolic BP > 180 mm Hg • diastolic BP >120 mm HgTaylor, DA. Hypertensive crisis: a review of the pathophysiology and treatment. Crit Care Clin N Am. 2015;27:439-447.
Hypertensive Urgency
•Acute increase in BP in the absence of symptoms suggesting acute organ damage: • Headache • Shortness of breath • Epistaxis• Usually noncompliant with prescribed medications or have not followed up and have not had their medications dosages titrated
quotesdbs_dbs2.pdfusesText_3 Images
Images